The measurement of clinic productivity was once fairly straightforward. The patient visit was the universally accepted unit of workload measure. Dividing total staff hours by clinic visits yielded staff hours per visit. Hours per visit could then be compared to budget, historical actuals, or industry average hours per visit. Alternatively, one could divide patient visits by the total number of provider FTEs and derive the average number of visits per clinician per 8-hour shift, expressed as visits per clinician FTE. This ratio could then be compared against budget, internally, or externally.
Today, measuring clinic productivity is more complicated. There are two issues that must be dealt with:
- The rise of non-visit patient work: emails, telephone consults, and other non-visit type encounters.
- The employment of physicians and the use of nurse practitioners.
Clinic Work Has Changed
Traditionally, patients visited the clinic and received treatment and the clinic billed for the visit. Today, clinics are exploring other options in which patients are assessed and given medical advice without having to visit. Where practical, it’s very efficient. Patients avoid having to go through registration and discharge. They avoid different layers of clinicians. They come in only when needing to be seen in person. For routine complaints – colds, flu, minor aches, etc. – having this kind of medical care as an option saves a lot of time for everyone. Clinics are encouraged to be more efficient, and yet they are penalized when their productivity measures do not reflect new operational practices.
Furthermore, not all clinic visits are the same. A flu shot involves less time and labor than treating a minor fracture and yet both are counted as visits with equal weight.
The better, more sophisticated, approach, is to count the direct labor time it takes for various types of visits and non-visit encounters. A five-minute inoculation is counted as five minutes. A one-hour appointment is counted as one hour. A 15-minute telephone consult is counted as 15 minutes. The total workload measure then becomes Direct Care Hours, as illustrated in the table below.
Physicians and Nurse Practitioners
Physicians under contract are usually separated out and analyzed separately. Separate or not, physicians and nurse practitioners spend different amounts of time per patient than allied health, schedulers, and billers. By treating these care providers as another skill level, we can assess their productivity along with everyone else. The template might look like this:
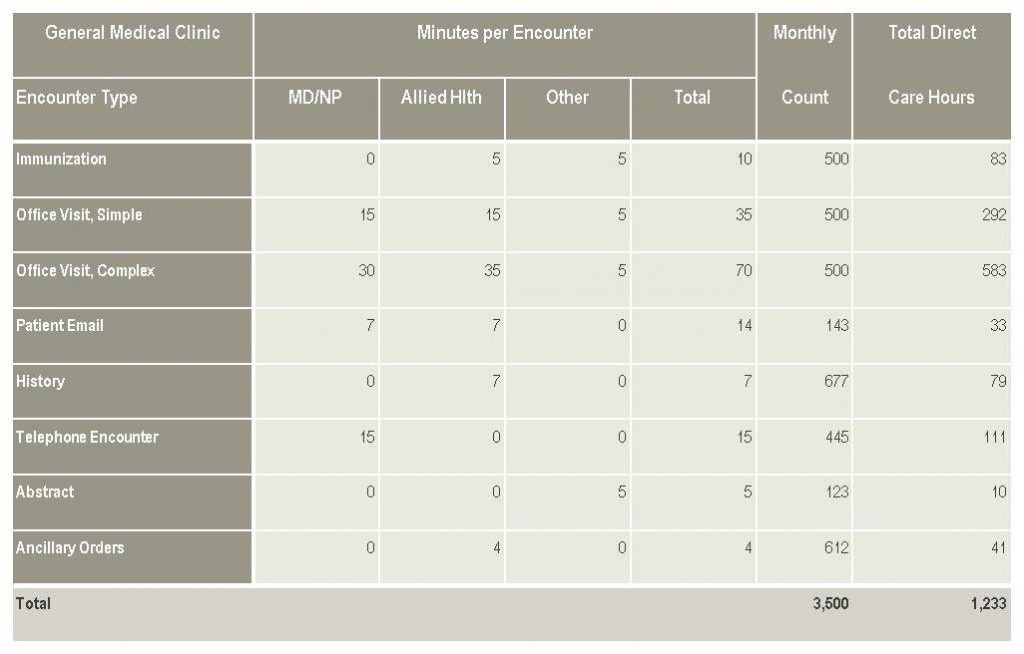
In this simple example, the various patient encounters types are captured, along with the direct hours of care necessary for a particular workload. Dividing Direct Care Hours by total hours worked in the clinic yields Hours Worked per Direct Care Hour, a productivity ratio that accounts for both patient volume and patient mix.
Healthcare is constantly evolving, as are patient care delivery systems. Physician-led clinics/Medical Groups are a large and growing segment of this system. As healthcare adopts an enterprise approach to managing costs and providing care we must develop methods to gauge productivity across the enterprise. Our industry will continue to change, and the pace of that change is showing no signs of slowing. Because of this we must continually examine our methods of tracking productivity to ensure they are effective and appropriate. __________________________________________________________________
Paul Fogel is President of Executive Information Systems, Inc., and author of Superior Productivity in Health Care Organizations: How to Get It, How to Keep It, Health Professions Press, 2003. He can be reached at Paul.Fogel@ExecutiveInfoSystems.com.